
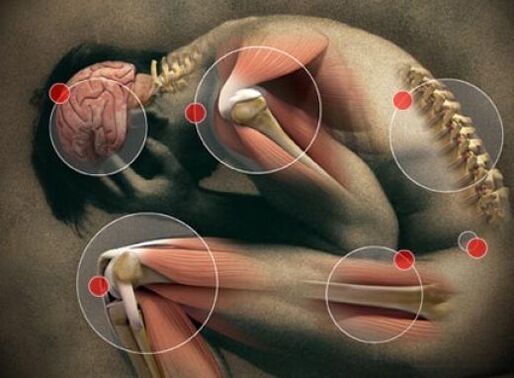
Joint pain- These are unpleasant sensations of pain and pulling in the joint area, the intensity of which sometimes reaches the level of pain. The symptom is combined with muscle pain, weakness, weakness, cracking, limited movement and may precede joint pain (arthralgia). Joint pain is accompanied by injuries to the musculoskeletal system, infections, diseases of the hematopoietic system and vascular pathology. Laboratory tests, ultrasound, x-rays, and invasive methods are used to identify the cause of the disorder. Treatment involves treating the disease that caused the pain.
Causes of joint pain
Mild or moderate joint discomfort is not always a manifestation of a pathological process. Sometimes the symptom has natural causes. Temporary joint pain is felt when wearing uncomfortable shoes and in weather-sensitive people, when the weather changes. During puberty, painful sensations in the shoulder and knee joints are due to insufficient blood supply due to accelerated bone growth.
Meaningful physical activity
During intense training or heavy work, a common cause of the symptom is overstrain of the musculoligamentous apparatus, less often it is caused by microtrauma of the cartilage and synovial membrane. A typical combination of joint pain and bone and muscle discomfort. Discomfort in the joints and muscles arise immediately after the impact. physical activity or in the context of prolonged monotonous work with constant tension on the same muscle groups. Pains in the joints of the body occur without fever. With large overloads, a moderate alteration of the general condition and weakness is possible.
The disorder can last up to several days and, with limited physical activity, gradually decreases until it disappears completely without any treatment. If aches and pains resulting from sports or intense physical work are replaced by persistent pain, swelling in the wrist, elbow, shoulder, ankle, knee and hip joints and limitation of usual movements, you should visit a doctor.
Age-related changes in the musculoskeletal system.
The causes of moderate pain in bones and joints in older people are degenerative processes with loss of calcium, thinning of the bone bundles, impaired blood supply to the cartilage and a decrease in the volume of intra-articular fluid. Mild discomfort is only the first manifestation of senile joint damage. Typically, periodic discomfort occurs after 45 to 50 years. At the age of 60-65, unpleasant pain occurs even with minor exertion, accompanied by stiffness of movement, bending, shuffling and gradually gives way to pain.
The pregnancy
Complaints about joint pain occur most often in the second half of gestational age. Painful pulling and discomfort is usually felt in the joints of the pelvis and lower extremities. It intensifies towards the end of the day, after standing for a long time or walking long distances. Night rest relieves the condition. Joint pain during pregnancy is due to the following reasons:
- Vitamin and mineral deficiency.. The most important role is played by calcium and vitamin D deficiency, which leads to osteomalacia. A characteristic of the manifestation of the symptom is a feeling of pain not only in the joints, but also in the bones, fatigue, the presence of other signs of hypocalcemia and hypovitaminosis D: cavities, brittle nails, muscle weakness, muscle pain and the appearance frequent ARVI.
- Significant weight gain. Joint discomfort is often a concern for pregnant women with significant weight gain or those who are obese. Pains at the end, and finally in the middle of the day, are felt in the hip, knee and ankle joints, whose cartilages experience loads several times higher than those allowed. To alleviate this condition, women deliberately limit physical activity, which leads to even faster weight gain.
- Softening of cartilage and ligaments.. Approximately half of pregnant women experience discomfort in the pelvic joints caused by the action of the hormone relaxin. In most cases, the discomfort consists of pain in the pubic area and hip joints. In a pathological course with the development of symphysitis, pain sensations are replaced by pain, which intensifies when pressing on the uterus, when trying to separate the legs, during sexual intercourse. The appearance of pain in the pubic area is a serious reason for visiting an obstetrician-gynecologist.
- Carpal tunnel syndrome. A specific manifestation found in the second or third trimester in almost 20% of pregnant women is the so-called tunnel syndrome. The cause of the disorder is swelling of the soft tissues of the hands and compression in the carpal tunnel of the nerves that pass to the fingers. In addition to pain in the small joints of the hand, patients complain of skin numbness, tingling and a tingling sensation. The condition improves with an elevated position of the arms.
Obesity
In overweight people, pressure on cartilage tissue increases, causing it to wear down more quickly. The degenerative-dystrophic process usually affects large joints of the lower extremities and intervertebral joints. The disorder increases as obesity progresses. Discomfort in the joints first manifests itself in the form of pain without fever at the end of the day, then the increasing destruction of cartilage leads to the development of deforming osteoarthritis, spondylosis, osteochondrosis with an acute pain syndrome that limits the patient's motor activity.
Acute infections
Body and joint pain is one of the first (prodromal) signs of many acute respiratory viral infections. The main causes of discomfort in the joints are intoxication of the body due to the spread of viruses and bacteria, the accumulation of toxins and the development of the inflammatory process. Usually, the patient complains that his entire body hurts, mild and moderate pain is observed in the joints, muscles and bones. The symptom is accompanied by weakness, fatigue, insomnia and frequent awakenings. Simultaneously with signs of pain and general malaise, chills and hyperthermia are observed.
The most pronounced pain in the joints and body occurs with the flu. Up to 50% of patients experience constant pain in the legs, arms and torso. The intensity of the pain is so high that it is difficult for a person to perform the simplest actions: get out of bed, go to another room, drink a glass of water. The situation is aggravated by high (febrile) temperature and severe headaches. Sore throat and nasal congestion appear after a few hours or even days. Less joint discomfort occurs with parainfluenza, an adenoviral infection.
It is possible to feel pain in the joints with acute infectious lesions of the gastrointestinal tract: infections due to food toxicities, salmonellosis. Joint pains of varying intensity appear suddenly a few hours after consuming contaminated food and are combined with a sharp increase in temperature, severe chills and headaches. The pain is preceded by nausea, vomiting, pain in the abdominal cavity, foul-smelling diarrhea with mucous and sometimes bloody impurities.
collagenous
Joint pain is a harbinger of most diseases that occur with autoimmune inflammation of connective tissue, including joint tissue. The localization, prevalence and intensity of unpleasant sensations are determined by the characteristics of a particular collagenosis. General patterns are the involvement of certain groups of joints in the process, a gradual increase in sensations up to unbearable and debilitating pain, observed first during movements and then at rest. Deformation of the articular joints is possible. The main systemic inflammatory causes of the disorder:
- Rheumatism. The symptom is "volatile": aching pains and then pain are in turn felt in the large joints of the arms and legs: elbows, shoulders, hips, knees and ankles. The affected areas are swollen. Joint discomfort is usually preceded by a sore throat. With treatment, joint changes are reversible.
- Rheumatoid arthritis. Unpleasant sensations usually appear after 40 years. Typical sensation of pain in the small joints of the hands and feet, combined with notable swelling and stiffness of movement in the morning. In the future, pain and curvature of the joints come to the fore.
- systemic scleroderma. It is characterized by a variable localization of pain sensations, the presence of stiffness in the morning in the joints of the hands, elbows and knees. The aches and pains are usually symmetrical. The swelling does not last long. Due to sclerosis of the skin, the mobility of the joints is limited, damage to the tendons causes a feeling of friction when moving.
Osteoarthritis
Pain syndrome in the initial stages of the disease is mild and is perceived as discomfort, pain in the joints of the legs and, less often, in the arms. The immediate cause of osteoarthritis is the degeneration and destruction of cartilage tissue. Typically, pulling or aching sensations without fever appear in adulthood and old age. Pain may begin earlier in the presence of occupational hazards (vibrations, heavy physical work). Gradually, the joints become stiff, the person experiences intense pain and difficulty walking and taking care of themselves.
Metabolic disorders
The causes of metabolic disorders in which joint pain occurs are an insufficient supply of vitamins, minerals, accelerated accumulation or excessive excretion of metabolic products. Unpleasant sensations are caused by inflammatory or dystrophic processes, have varying severity and, in most cases, serve as a manifestation of pathological conditions such as:
- Osteoporosis. When calcium is removed from bone tissue, the articular surfaces of bones become brittle and cartilage becomes thinner, which is accompanied by painful sensations. The pain syndrome gradually increases from mild pain to severe arthralgia, combined with unpleasant sensations in the bones and muscle weakness. The joints that experience the maximum load are the most affected: the hip and knee; the shoulder, elbow and ankle are less commonly affected.
- Drop. Slight pain in the big toe is already a cause for concern in the preclinical stages of the gouty process. There may be discomfort in the knees, elbows, wrists and fingers. The accumulation of urates in the joint cavity leads to a rapid manifestation of the disease with a change from pain to acute painful joint pain that does not go away for several hours. The affected joint is warm to the touch. There is redness of the skin and limited movement.
Oncological diseases
In acute and chronic leukemia, generalized osteoarticular pains, followed by pain, often occur even before pathological changes are noted in a general blood test and other clinical symptoms: malaise, night sweats, fever, loss of appetite, bleeding. Unpleasant sensations at first are periodically painful, then constantly strong and weaken the patient.
Hodgkin's lymphoma and lymphogranulomatosis are characterized by a combination of joint pain with muscle discomfort, weakness, enlarged lymph nodes and other lymphoid formations. Pain sensations are common, usually moderate. In osteosarcomas, a short period of pain in the knee joint and thigh muscles is observed, which intensifies at night and with exertion turns into constantly increasing pain with limping. Other joints are less affected by this pathology.
Joint injuries
Joint pain is caused by mild traumatic injuries, which cause damage to the ligaments surrounding the joint and bruising of the soft tissues in the joint area. More intense pain occurs when the meniscus is damaged. The symptom is clearly related in time to a blow, a fall or a clumsy movement. Discomfort is usually felt in an affected joint and, less commonly, spreads to adjacent areas of the body.
Chronic infectious processes
Possible causes of a feeling of pain in the joints that occurs without fever or against the background of low-grade fever are long-term infections. In patients suffering from chronic infectious and inflammatory diseases, discomfort in the joints becomes a consequence of intoxication of the body or the direct harmful effects of microorganisms on the tissue of the joints (usually streptococci, mycoplasmas, chlamydia). The appearance or intensification of pain may indicate an exacerbation of chronic tonsillitis, sinusitis, genitourinary infections, adnexitis, pyelonephritis.
Distinctive features of joint pain in common chronic infections occurring with poisoning are moderate severity of joint discomfort, gradual development, periodic intensification and weakening of symptoms. In patients suffering from tuberculosis and hematogenous osteomyelitis, the background of the development of painful sensations is an increase in temperature to subfebrile levels, general malaise: fatigue, weakness, weakness. Without treatment, patients' condition progressively worsens.
Complications of pharmacotherapy.
Taking some medications can be complicated by moderate pain and discomfort in the small joints of the hands. The unpleasant sensations are not accompanied by redness or deformation of the joints. Patients may complain of muscle pain, fever, skin rashes, and other manifestations of drug allergies. Discomfort disappears quickly after stopping the medication that caused it, and special treatment is less likely to be required for complications that arise. Mild pain and arthralgia are caused by:
- antibiotics: penicillins, fluoroquinolones.
- Tranvilizers: phenazepam, diazepam, lorazepam, etc.
- Contraceptives: combined oral contraceptives (COCs).
rare causes
- Inflammation of the respiratory system. : pneumonia, bronchitis, tracheitis.
- intestinal pathology: nonspecific ulcerative colitis, Crohn's disease.
- skin diseases: psoriasis.
- Endocrine disorders: diabetes mellitus, diffuse toxic goiter, hypothyroidism, Itsenko-Cushing disease.
- Autoimmune processes: Hashimoto's thyroiditis, vasculitis.
- fascial damage: necrotizing fasciitis in the convalescent stage.
- Congenital defects of bones and joints..
Survey
To determine why pain is felt in the joints and bones, it is necessary to consult a therapist or family doctor, who will make an initial diagnosis and prescribe examinations carried out by specialized specialists. Taking into account the nature of the unpleasant sensations, the speed of their appearance and the accompanying symptoms, the following is recommended to determine the cause of the disorder:
- laboratory blood test. An evaluation of the leukocyte count and ESR level is required to exclude infections, inflammatory and oncohematological processes. In systemic diseases, it is important to measure the content of total proteins, the ratio of protein fractions in the blood, specific acute phase proteins, markers of rheumatoid arthritis and other inflammations. Tests for concentrations of vitamins, electrolytes (especially calcium), and uric acid help diagnose metabolic disorders.
- bacteriological examination. Bacterial culture is necessary if the pains felt in the joints and throughout the body are likely to be infectious. For research, urine, feces, sputum and secretion from the urogenital tract are collected. To select an antimicrobial therapy regimen, antibiotic sensitivity is determined. In doubtful cases, microscopy and culture are complemented by serological reactions (RIF, ELISA, PCR).
- Ultrasound of articular joints.. Usually it is used for clear localization of painful sensations and suspicion of rheumatic diseases. Ultrasound of the joint allows us to examine its structure, identify cartilage and bone destruction, preclinical inflammatory changes, and study the state of periarticular soft tissues. The advantages of the method are accessibility, non-invasiveness and high information content.
- x-ray techniques. During joint x-rays, changes in the width of the joint space, hardening of soft tissues, the presence of calcifications, osteophytes and erosions of the joint surfaces are detected. To improve the effectiveness of diagnosis, special techniques are used: contrast arthrography, pneumoarthrography. In the initial stages of injury, tomography (MRI, CT of the joints) is considered more indicative. Bone density can be conveniently assessed using densitometry.
- Invasive examination techniques.. In some cases, to determine the cause of joint pain, a puncture with a biopsy of the cartilage, the inner lining of the synovial membrane and tophi is performed. Morphological analysis of biopsy samples and examination of synovial fluid reflect the nature of pathological processes occurring in the joints. It is convenient to carry out simultaneous collection of materials with a visual examination of the joint cavity during arthroscopy with tissue biopsy.
A less common way to diagnose the cause of joint pain is scintigraphy with the introduction of technetium, which accumulates in the affected tissues. In recent years, there has been increasing interest in joint thermography as a modern non-invasive method to recognize inflammatory diseases, tumors and circulatory disorders in the joints and periarticular tissues. If the number of elements formed in a clinical blood test decreases, extra-articular bone puncture is performed. Patients with joint pain without fever are recommended to consult a rheumatologist and orthopedic traumatologist.

Treatment
Help before diagnosis
For joint pain associated with physical activity, no special treatment is required, prolonged rest with dosage of loads is sufficient. Unpleasant sensations in the joints that occur during pregnancy usually disappear on their own after pregnancy or are corrected by controlling weight and taking vitamin and mineral supplements. Elderly and obese patients are advised to change their lifestyle: adequate physical activity, a diet with adequate calorie content and sufficient content of plant foods.
Pain in the bones, joints and muscles, combined with general malaise and fever, an increase in the sensation of pain and pulling to the point of severe pain, and the development of persistent pain are indications to consult a doctor. To reduce joint discomfort caused by ARVI, it is recommended to rest, drink enough water, rosehip infusions and dried fruits. Until serious diseases that cause pain in the joints, self-medication with painkillers, prolonged and unsuccessful application of compresses, lotions, decoctions, etc. are excluded. , are unacceptable.
Conservative therapy
You can get rid of joint pain with proper treatment, aimed at eliminating the cause of the disorder and individual parts of the mechanism of its development. Etiopathogenetic therapy is usually complemented by symptomatic medications that quickly reduce the severity of persistent and aching pain. The treatment regimen for diseases that occur with joint pain may include:
- Antimicrobials. The basic therapy for infections is based on the prescription of antibiotics to which the pathogen is susceptible. In severe cases, broad-spectrum drugs are used until the sensitivity of the microorganism is established.
- Non-steroidal anti-inflammatory drugs. They reduce the production of inflammatory mediators and therefore inhibit inflammatory processes in the joints. By influencing central pain receptors, they reduce the degree of joint discomfort. Used in the form of tablets, ointments, gels.
- corticosteroids. They have a strong anti-inflammatory effect. Hormonal therapy is the basis for the treatment of systemic collagenosis. In severe and resistant forms of the disease, corticosteroids are combined with immunosuppressants to enhance the effect.
- Chondroprotectors. They act as a substrate for the synthesis of protein glycans, a sufficient amount of which increases the elasticity of articular cartilage. Nourishes cartilage tissue and restores its damaged structure. Intra-articular administration of drugs is possible.
- Xanthine oxidase inhibitors. Used as anti-gout drugs. They block the key enzyme necessary for the synthesis of uric acid, thereby reducing its concentration in the body and promoting the dissolution of existing urate deposits.
- Vitamin and mineral complexes.. Recommended for the treatment of joint pain caused by metabolic disorders. The most commonly used drugs contain calcium and vitamin D. They are also an element of complex therapy for inflammatory and metabolic diseases.
- Chemotherapeutic agents. They serve as the basis for most treatment regimens for various types of oncohematological pathologies. Depending on the clinical variant and severity of the neoprocess, they are combined with radiotherapy and surgical interventions.
Physiotherapy
Once the exact cause of the pain is identified and the acute inflammation subsides, patients, except those suffering from cancer, are prescribed physical therapy and exercise therapy. Microwave and ultrasound therapy sessions, electrophoresis and pulsed currents have a good anti-inflammatory and analgesic effect. In case of chronic pathology, physiotherapy treatment is carried out for several months and is complemented by spa therapy.
































